Immunotherapy: A Breakthrough in Fighting Against Cancer
According to the Centers for Disease Control and Prevention, cancer is the second leading cause of death in the US. Similarly, the National Cancer Institute reports that approximately 38.9% of people will be diagnosed with cancer at least once in their lives. (2021) With such large numbers of people currently affected and set to be diagnosed with cancer in the future, there is a race against time to find plausible treatments to fight advancing cancer. Common treatments in today’s cancer aversion efforts include surgery, chemotherapy, and radiation therapy. Recently, though, there has been a surge in immunotherapy. This promising form of cancer treatment has been shown to have multiple strategic advantages in combating this evolving disease. However, how did this therapy emerge, how is it used today, and what can we expect to find in the future?
Immunotherapy and Cancer:
To understand treatments against cancer, it’s important to first learn what this disease is. The National Cancer Institute coined cancer as “a disease in which some of the body’s cells grow uncontrollably and spread to other parts of the body.” (2025) In reality, cancer is so much more complex than its definition. The primary reason why cancer doesn’t have a “cure” and needs multiple types of treatments to suppress its evolution lies within its complex nature. It isn’t a disease that attacks from the outside; it’s a disease created through mutations and cell dysfunction. According to the Worldwide Cancer Research Organization, cancer arises from cell mutations and it varies differently on a genetic and molecular level for different people. (2025)
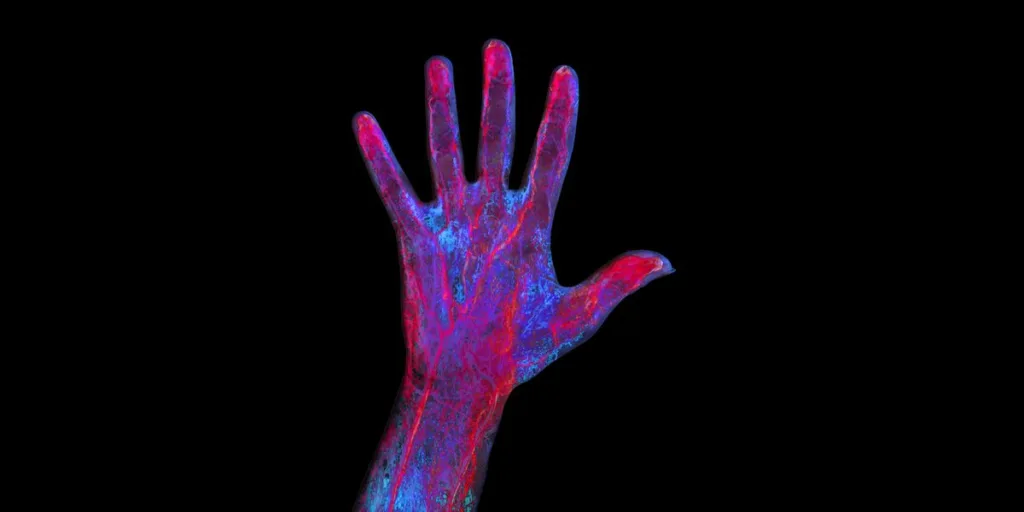
Cancer isn’t a “one-size-fits-all” disease; due to its inherently complex nature, different variations of cancer pose difficulty when attempting to find a “cure.” One form of treatment, which has revolutionized cancer treatment for patients, is immunotherapy. Immunotherapy is a biologic therapy that uses and evokes the patient’s immune system to fight cancer. (UVA Health, n.d.) However, at a deeper level, immunotherapy operates the way cancer does. Similar to cancer, immunotherapy is a broad spectrum that doesn’t have a singular function. According to the Dana-Farber Cancer Institute, immunotherapy treatments work in a multitude of ways depending on the patient’s needs. (2025) One of its pathways is training the immune system to recognize and attack specifically cancer cells, since those cells often present themselves as harmless, which leads the immune system to initially restrict itself from attacking the cancer cells. (Dana-Farber Cancer Institute)
History of Immunotherapy
Immunotherapy has risen in popularity in recent decades as a tool to fight against cancer. However, the concept of immunotherapy to fight cancer has existed for centuries. According to Dobosz and Dzieciątkowski, as early as Ancient Egypt to the 19th century, scientists were able to observe a pattern: tumors would disappear when the patient was infected with high fevers. (2019) Such observations yielded a common consensus: when the immune system attacks an infection or fever, it also ends up eliminating cancer cells. William Coley, who was known as the father of immunotherapy, was one of the first to use these observations in an experiment by using the immune system to treat bone cancer in 1891. Through many case observations, he was able to understand that when a patient with an “incurable” cancer was infected with a bacterial infection, the patient went into spontaneous remission. (Dobosz & Dzieciątkowski, 2019) Furthermore, Coley took his research into an experimental direction by injecting various diseases directly into tumors, subsequently creating the first immunotherapy cancer treatment. Since then, interest in utilizing immunotherapy has skyrocketed, with multiple scientists exploring and experimenting with the potential benefits of using immunotherapy on difficult-to-treat cancers.
Current Usage of Immunotherapy
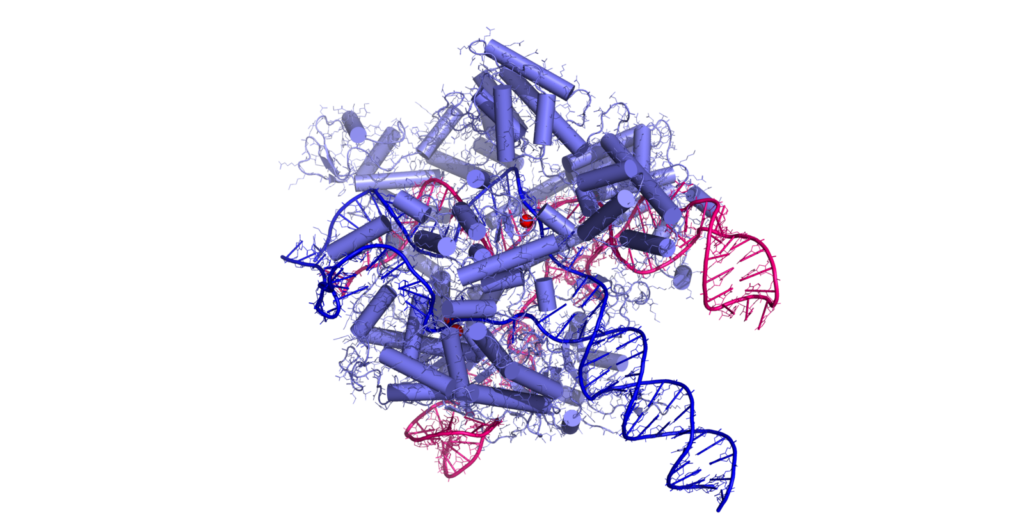
In recent years, immunotherapy hasn’t been used to fight all cancers; its potency lies in its unique approach in fighting specific cancer cells, thus potentially eradicating cancer. Common treatment options such as radiation therapy and chemotherapy eliminate cells in the general vicinity where the cancer is located. However, this poses a detrimental flaw; cancer can return since those types of treatment don’t directly target cancer cells. In recent decades, scientists have evolved immunotherapy as a form of treatment in which they “train” the immune system to identify and attack specific cancer cells, leading to the potential eradication of cancer. According to Zhang and Chen, oftentimes, cancer cells trick immune checkpoints by activating them, therefore signaling to the immune system that those cells are safe. (2018) Therefore, the current research standpoint is aimed at blocking these checkpoints so that the immune system can identify those cancer cells and attack. This process is made possible through engineered T cell therapy. (Zhang & Chen, 2018) Aside from checkpoint inhibitors, more common usage of immunotherapy is using “Monoclonal Antibodies” to help the immune system target and kill cancer cells and “Adoptive T Cell Therapy” (ACT) where T-cells (a type of immune cell) are genetically developed in a lab and reintroduced to kill cancer cells. (Zhang & Chen, 2018)
Conclusion
Cancer is an ever-evolving disease, one that we may never get rid of. Through medical advancements in treatments such as immunotherapy, we get one step closer to saving lives and preventing deaths. To fight this evolving disease, we must evolve our treatments to identify and fight cancer cells and tumors. Immunotherapy, a form of revolutionary therapy that was recognized for its ability to evolve and fight specific types of cancer cells, has the potential to do more. By pairing immunotherapy with medical innovations such as CRISPR and adoptive T-cell therapy, we can further our advancements and create faster and more effective cures for cancer.
References
Centers for Disease Control and Prevention (2024). Leading Causes of Death, United States. Retrieved from https://www.cdc.gov/womens-health/lcod/index.html
Dana-Farber Cancer Institute (n.d.). Immunotherapy https://www.dana-farber.org/cancer-care/treatment/immuno-oncology/immunotherapy#:~:text=What%20is%20Immunotherapy?,is%20disabled%20in%20your%20browser
Dobosz, P., & Dzieciątkowski, T. (2019). The Intriguing History of Cancer Immunotherapy. Frontiers in immunology, 10, 2965. https://doi.org/10.3389/fimmu.2019.02965
National Cancer Institute (2025). Cancer Statistics.
https://www.cancer.gov/about-cancer/understanding/statistics
UVA Health (n.d.). Immunotherapy for Cancer Treatment. https://uvahealth.com/services/cancer/immunotherapy
Worldwide Cancer Research (2025). Why is cancer so hard to cure?
Zhang, H., & Chen, J. (2018). Current status and future directions of cancer immunotherapy. Journal of Cancer, 9(10), 1773–1781. https://doi.org/10.7150/jca.24577