In August 2024, a boy named KJ Muldoon was born. He wasn’t a normal, healthy baby, though. He had a genetic disorder called a CPS1 deficiency that made it difficult for him to process protein. This simple fact is dangerous in itself, but it also makes him have a lot of ammonia in his blood. Too much ammonia is toxic to the brain, so this disorder is extremely deadly.
However, when he was born, a team of scientists from around the world rallied together to create a personalized gene therapy for him. This first of its kind treatment was given to him when he was six months old. After getting three separate doses of this treatment to edit his genes, the mutation seems to be fixed. This was an incredible process that could revolutionize the future of healthcare.
How was this treatment developed?
When KJ was first born with this disorder, scientists got right to work. They took steps to create this treatment that usually takes almost 10 years, but they collaborated and got it done in just a few months. In most cases, the only way to treat his disease is to get a liver transplant, but it would be a long time before he would be able to get one. This causes 50% of babies with this disease to die before getting a transplant.
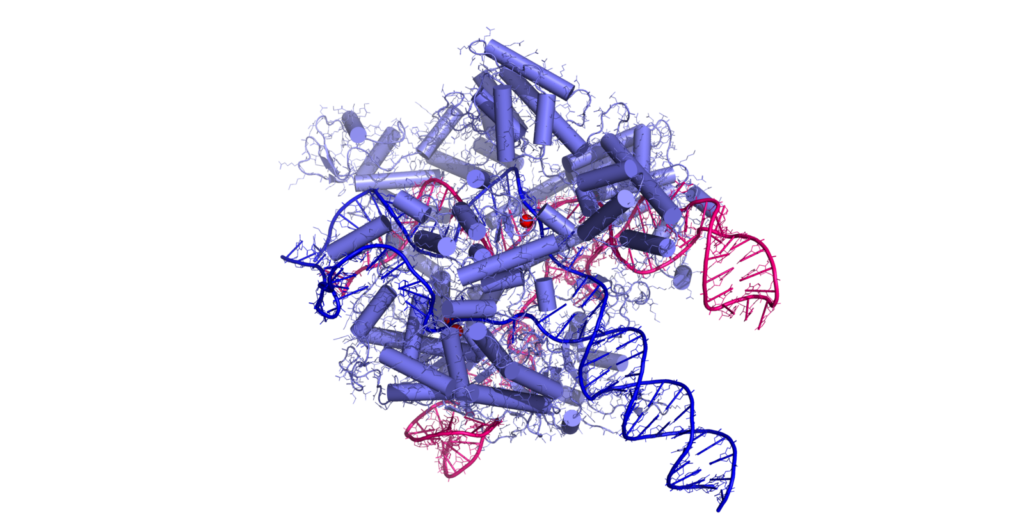
So, the scientists got the parents’ permission to use base editing to try and fix the mutation. Base editing is when they make selective changes to single-letters in DNA sequences. For the base editing approach, fatty lipid molecules were wrapped around a treatment to stop it from breaking down in his blood when it was travelling to his liver, where it made the edit. The lipids housed instructions on how the cells should create an enzyme that can then change the gene. Also, they bring CRISPR with them, which finds the exact letter in the DNA that has to be changed.
This treatment was actually possible because of decades of federally funded research into things like CRISPR technology. CRISPR is an acronym for Clustered Regularly Interspaced Short Palindromic Repeats. It’s part of the immune system of bacteria that cuts DNA and we now use it as a kind of molecular scissors to edit genes. There are two parts of this system. First, there’s a CRISPR-associated nuclease whose job is to connect and cut DNA. There’s also the guide RNA sequence whose job is to direct the CRISPR-associated nuclease so it reaches its target. This whole process lets scientists rewrite an organism’s genetic code and do things like create drought-resistant crops.
They had to use this CRISPR technology to personalize KJ’s treatment because, with CPS1 deficiency being a rare disease, pharmaceutical companies are not willing to spend several years and millions of dollars to develop a large-scale treatment. Also, a lot of the time different mutations cause each individual’s disorder, so a mass produced product would possibly not be as effective as this treatment ended up being.
In fact, after just his first dose, KJ was able to safely eat as much protein as he was supposed to at his age. He continued getting treatments to get his ammonia levels under control and, after only three doses, he was done with the treatment. Now, he is almost a year old, and while scientists are still cautious to call his disorder cured and do not know if he will still need a liver transplant someday, KJ does seem to be doing very well right now.
Implications for the future
This promising sign could lead to a brighter, healthier future for society. First of all, CRISPR could be used in the future to treat other extremely uncommon genetic diseases. The problem with this gene editing therapy though is that it is extremely expensive, so it would not be a cost-effective solution for most people with these issues. At the same time, now that they’ve treated KJ, they can adapt his treatment to fix other people’s mutations too. That means that future treatments could be cheaper for people.
Even though it seems to have been successful so far, this one personalized treatment took teams of scientists and months of work to pull off. Logistically, this would be impossible to do for everyone with a rare disorder. The possibility of this treatment however does create new possible futures, like one where cystic fibrosis or Huntington’s disease could have a form of treatment.
Despite all the potential financial issues, personalizing gene therapy will inevitably save lives. People with rare diseases will have more of a chance at survival, and in the future, the technology will develop and likely become more accessible. The success of baby KJ’s treatment is a promising step towards a future where certain genetic disorders are no longer a death sentence, but, instead, with some work done by scientists, they will just be another part of their long, healthy lives.
References
Kolata, G. (2025, May 15). Baby Is Healed With World’s First Personalized Gene-Editing Treatment. The New York Times. Retrieved June 7, 2025, from https://www.nytimes.com/2025/05/15/health/gene-editing-personalized-rare-disorders.html
Ledford, H. (2025, May 15). World’s first personalized CRISPR therapy given to a baby with genetic disease. nature. Retrieved June 7, 2025, from https://www.nature.com/articles/d41586-025-01496-z
What is CRISPR: The Ultimate Guide to CRISPR Mechanisms, Applications, Methods & More. (n.d.). Synthego. Retrieved June 7, 2025, from https://www.synthego.com/learn/crispr